Blood Sugar Basics
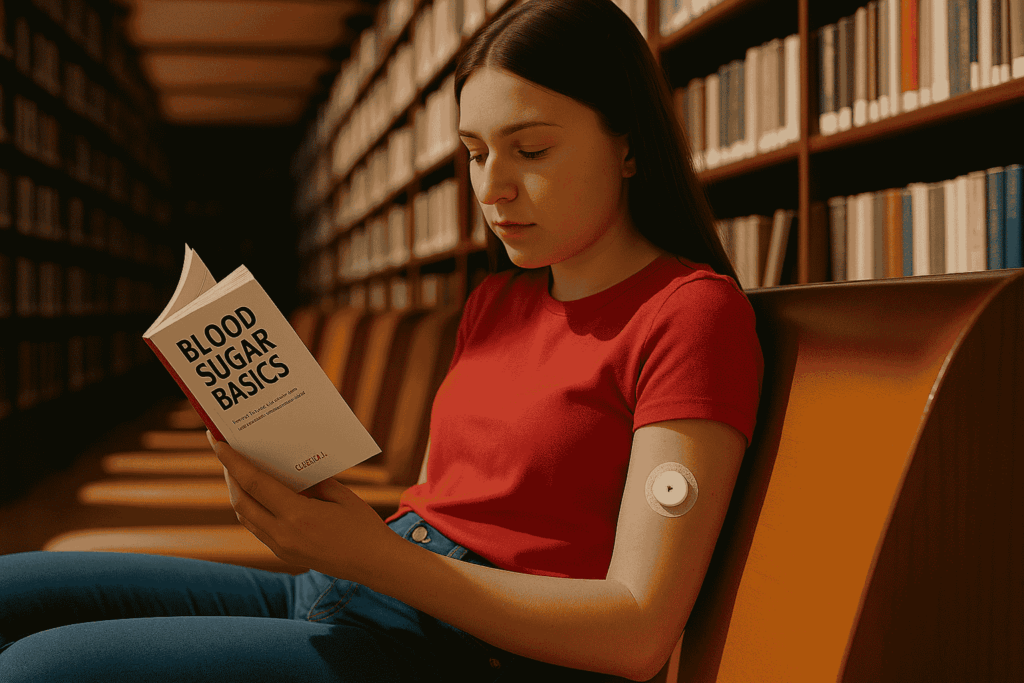
Understanding blood sugar levels is like learning to read your body’s vital signs. For people with Type 1 Diabetes, knowing what’s “high,” what’s “low,” and how to recognize the warning signs can make the difference between feeling great and facing a medical emergency. But here’s the good news: with practice and knowledge, managing blood sugar becomes second nature.
Whether you’re newly diagnosed, supporting someone with T1D, or simply want to sharpen your skills, this guide will help you master the fundamentals of blood sugar management and feel confident in recognizing when action is needed.
What Are Normal Blood Sugar Ranges?
Blood sugar (glucose) levels fluctuate throughout the day based on food, activity, stress, illness, and insulin. Understanding target ranges helps you know when levels are safe versus when they need attention.
Target Blood Sugar Ranges for People with T1D:
General Adult Targets:
- Fasting (before meals): 80-130 mg/dL
- 2 hours after meals: Less than 180 mg/dL
- Bedtime: 100-140 mg/dL
- A1C goal: Less than 7% (varies by individual)
Pediatric Targets (may vary by age):
- Before meals: 90-130 mg/dL
- Bedtime: 90-150 mg/dL
- A1C goal: Less than 7.5% (varies by age and individual circumstances)
Important Note: Your healthcare provider may set different targets based on your age, health conditions, hypoglycemia awareness, and individual circumstances. Always follow your personalized goals.
Understanding Blood Sugar Classifications
Normal/Target Range (70-180 mg/dL):
- Optimal range for most daily activities
- Body functions normally
- Energy levels stable
- No immediate intervention needed
Hypoglycemia (Low Blood Sugar – Below 70 mg/dL):
- Requires immediate treatment
- Can be dangerous if untreated
- Symptoms often develop quickly
- May impair judgment and coordination
Hyperglycemia (High Blood Sugar – Above 180 mg/dL):
- Needs attention but usually not immediately life-threatening
- Can cause long-term complications if frequent
- May require insulin correction
- Symptoms develop more gradually
Severe Hypoglycemia (Below 54 mg/dL):
- Medical emergency requiring immediate treatment
- May cause unconsciousness or seizures
- Requires glucagon or emergency medical care
- Should always be followed up with healthcare provider
Recognizing Low Blood Sugar (Hypoglycemia)
Low blood sugar can develop quickly and requires immediate action. The key is learning to recognize your personal warning signs and acting fast.
Early Warning Signs:
- Shakiness or trembling
- Sweating (especially sudden, unexplained sweating)
- Hunger, even if you recently ate
- Irritability or sudden mood changes
- Rapid or irregular heartbeat
- Dizziness or lightheadedness
- Difficulty concentrating
- Fatigue or weakness
Moderate Symptoms:
- Confusion or difficulty thinking clearly
- Blurred vision
- Headache
- Nausea
- Feeling anxious or nervous
- Pale skin
- Clammy or cold skin
- Coordination problems
Severe Symptoms (Medical Emergency):
- Severe confusion or disorientation
- Slurred speech
- Loss of consciousness
- Seizures
- Inability to eat or drink
- Combative or aggressive behavior
Individual Symptom Patterns: Everyone experiences hypoglycemia differently. Some people feel shaky first, while others notice mood changes or hunger. Keep a log of your symptoms to identify your personal warning signs.
What Causes Low Blood Sugar?
Understanding the common causes helps you prevent hypoglycemia and recognize high-risk situations:
Common Triggers:
- Too much insulin for the amount of food eaten
- Skipping meals or eating later than usual
- Increased physical activity without adjusting insulin or food
- Alcohol consumption (especially on an empty stomach)
- Illness or vomiting
- Hot weather or baths/showers
- Stress or emotional factors
- Menstrual cycle changes
- Sleep deprivation
High-Risk Times:
- 1-3 hours after taking rapid-acting insulin
- During or after exercise
- Between meals if meal timing is delayed
- Overnight (especially 2-4 AM)
- During illness or when not eating normally
Treating Low Blood Sugar: The Rule of 15
When blood sugar drops below 70 mg/dL, follow this proven treatment protocol:
Step 1: Consume 15 grams of fast-acting carbohydrates
- 4 glucose tablets
- 1/2 cup (4 oz) of fruit juice
- 1/2 cup regular (not diet) soda
- 1 tablespoon honey or sugar
- 3-4 pieces of hard candy
Step 2: Wait 15 minutes
- Avoid the urge to eat more immediately
- Stay seated or lie down if feeling dizzy
- Avoid driving or operating machinery
Step 3: Recheck blood sugar
- If still below 70 mg/dL, repeat treatment
- If above 70 mg/dL, eat a snack with protein and carbs
Step 4: Follow up
- Have a snack if your next meal is more than 1 hour away
- Monitor blood sugar more frequently for the next few hours
- Document the episode and discuss patterns with your healthcare team
For Severe Hypoglycemia:
- If unconscious or unable to swallow: Use glucagon injection
- Call 911 for emergency medical help
- Never force food or liquid into an unconscious person’s mouth
- Position person on their side to prevent choking
Recognizing High Blood Sugar (Hyperglycemia)
High blood sugar develops more gradually than low blood sugar, but it’s equally important to recognize and address.
Early Signs:
- Increased thirst
- Frequent urination
- Fatigue or drowsiness
- Blurred vision
- Headache
- Difficulty concentrating
- Dry mouth
Moderate Symptoms:
- Nausea or stomach discomfort
- Shortness of breath
- Weakness
- Confusion
- Flushed, dry skin
- Rapid heartbeat
- Drowsiness
Severe Symptoms (Diabetic Ketoacidosis – DKA):
- Vomiting
- Abdominal pain
- Fruity breath odor
- Rapid, deep breathing
- Severe dehydration
- Unconsciousness
- This is a medical emergency requiring immediate hospital care
What Causes High Blood Sugar?
Common Triggers:
- Eating more carbohydrates than usual
- Missing insulin doses or taking too little insulin
- Illness or infection
- Stress (physical or emotional)
- Certain medications (steroids, some antibiotics)
- Lack of physical activity
- Insulin that has expired or been stored improperly
- Hormonal changes (growth spurts, menstruation, pregnancy)
- Dehydration
Dawn Phenomenon: Many people experience higher blood sugar in the early morning hours due to natural hormone releases. This is normal and can be managed with adjusted insulin timing or doses.
Managing High Blood Sugar
Immediate Actions:
- Check blood sugar to confirm the reading
- Check for ketones if blood sugar is above 250 mg/dL
- Take correction insulin as prescribed by your healthcare provider
- Drink water to stay hydrated
- Avoid exercise if ketones are present
When to Seek Medical Help:
- Blood sugar above 400 mg/dL
- Moderate to large ketones in urine or blood
- Vomiting and unable to keep fluids down
- Signs of dehydration
- Difficulty breathing or chest pain
- Confusion or altered mental state
Prevention Strategies:
- Take insulin as prescribed
- Monitor blood sugar regularly
- Stay hydrated
- Maintain regular meal timing
- Manage stress effectively
- Get adequate sleep
- Keep insulin properly stored
The Role of Continuous Glucose Monitoring
Benefits of CGMs:
- Real-time blood sugar readings
- Trend arrows showing if levels are rising or falling
- Alerts for impending highs and lows
- Data sharing with family and healthcare providers
- Reduced need for fingerstick tests
Understanding CGM Readings:
- Trend arrows are as important as the number
- Calibration may be needed with some systems
- Compression lows can occur when lying on the sensor
- 15-minute delay compared to fingerstick readings
CGM Alerts:
- Low glucose alarms (typically set at 70 mg/dL)
- High glucose alarms (typically set at 180-200 mg/dL)
- Rapid rate-of-change alerts
- Predicted low alerts (30 minutes in advance)
Blood Sugar Patterns and Timing
Pre-Meal Testing:
- Helps determine insulin dosing
- Should be done 15-30 minutes before eating
- Indicates how well previous meal was managed
Post-Meal Testing:
- Check 2 hours after eating
- Shows how well insulin matched food intake
- Helps identify foods that cause spikes
Bedtime Testing:
- Ensures safe overnight levels
- May require snack if too low
- Helps prevent overnight hypoglycemia
3 AM Testing:
- Recommended occasionally to check for overnight lows
- Helps identify dawn phenomenon
- Important for adjusting long-acting insulin
Special Situations
During Exercise:
- Check blood sugar before, during, and after activity
- Levels may drop hours after exercise
- Reduce insulin or increase food intake as needed
- Stay hydrated and monitor for delayed hypoglycemia
When Sick:
- Blood sugar often runs higher during illness
- Continue taking insulin even if not eating
- Check blood sugar and ketones more frequently
- Stay hydrated and contact healthcare provider if levels remain high
During Stress:
- Emotional and physical stress can raise blood sugar
- Monitor levels more frequently during stressful periods
- Use stress management techniques
- Adjust insulin as needed with healthcare provider guidance
Building Blood Sugar Awareness
Keeping a Log:
- Record blood sugar readings, insulin doses, food intake, and symptoms
- Note patterns and triggers
- Share with healthcare provider at appointments
- Use smartphone apps for easy tracking
Symptom Recognition:
- Pay attention to how you feel at different blood sugar levels
- Some people lose hypoglycemia awareness over time
- Regular blood sugar checks help maintain awareness
- Discuss concerns with your healthcare team
Family and Friends:
- Teach close contacts to recognize symptoms
- Ensure they know how to help during emergencies
- Keep glucagon and emergency supplies accessible
- Practice emergency scenarios together
Final Thoughts
Mastering blood sugar basics is one of the most empowering skills you can develop in managing Type 1 Diabetes. While it may seem overwhelming at first, remember that millions of people successfully manage their blood sugar levels every day and live full, active lives.
The key is consistent monitoring, recognizing your personal patterns, and taking prompt action when needed. Every person with T1D has unique responses to food, insulin, exercise, and stress, so be patient as you learn what works best for your body.
Trust your instincts—if something feels off, check your blood sugar. Technology like CGMs can be incredibly helpful, but they’re tools to support your knowledge and awareness, not replace them.
With time, practice, and the right support from your healthcare team, managing blood sugar becomes as natural as checking the time. You’re building skills that will serve you well throughout your journey with T1D.
Remember, you’re not aiming for perfection—you’re aiming for safety and the best possible quality of life. Every blood sugar check, every treatment of a low, and every adjustment you make is an investment in your health and future.
You’ve got this, and you’re never alone in this journey.
